Introduction and objective
Updated AUA/SUFU guidelines for the evaluation of microhematuria (MH) were released in May 2020. These guidelines recommend stratification based on patient risk factors to direct diagnostic testing. Questions remain as to whether current divisions between risk groups accurately reflect difference in cancer risk, especially among women. Objectives of the current study are to 1) determine the prevalence of urologic malignancy in women evaluated for MH in a large university-based urology practice, 2) describe clinical features shared by women with MH, and 3) evaluate a risk score for urologic malignancy in women with MH.
Methods
A retrospective chart review identified women with MH evaluated by a large, university-based urology practice between 2010 and 2020. Clinical and demographic variables associated with their evaluation, referral pattern, appropriateness of referral and evaluation, workup completed, and resulting diagnoses were reported. Patterns of repeat evaluations were also described. Patients were stratified as low, intermediate, or high risk according to AUA/SUFU recommended risk stratification.
Results
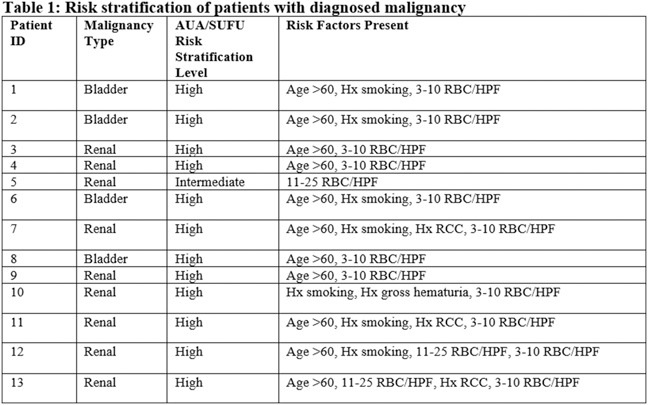
4456 charts resulted from an initial query based on females with ICD-9 and ICD-10 codes for MH between 2010-2020. 1730 patients (95.5% referrals v. 4.5% established urology patients) met criteria for inclusion in the study, and 1350 underwent evaluation for MH at the practice. Over 30% of referrals were considered inappropriate. 13 patients were diagnosed with urologic malignancy, all of whom were classified as intermediate- or high-risk according to AUA/SUFU criteria. Over 10% of patients had at least 2 evaluations for MH, with only 1 malignancy discovered on repeat evaluation for persistent MH.
Conclusions
Inappropriate referrals for MH are common. Incidence of urologic malignancy is incredibly low among women evaluated for MH, but especially among those classified as “low risk” by new guidelines. Repeated evaluations for persistent, stable MH appear low yield in detecting malignancy.
Source of Funding
The authors express gratitude to the Emory Department of Urology for research pilot grant funding, which made this research possible